A Structured Medical History will be required and any obvious trigger event for the plantar fasciitis, like a fall, or a change in exercise like couch to 5KM.
Most cases of Plantar Fasciitis do not have an easily identifiable trigger event or trauma.
Physical Examination Techniques
The physical examination aims to confirm the clinical suspicion of plantar fasciitis, assess biomechanical contributors, and exclude alternative diagnoses. Key components include inspection, palpation, range of motion, strength testing, functional assessment, and special tests.
Inspection of feet
- Gait observation: walking gait, altered foot strike, or compensatory patterns.
- Posture and foot type: Flat feet, high arches, or abnormal pronation/supination.
- Swelling, erythema, or bruising: Uncommon in plantar fasciitis; may suggest alternative issues pathology.
- Footwear assessment: Wear patterns, support, and fit.
Hands On
- Maximal tenderness at the heel of foot at the plantar fascia insertion is highly suggestive.
- Plantar fascia: Pressure along its length for focal or diffuse tenderness.
- Fat pad, calcaneus, and arch: Assess for atrophy, masses, or bony abnormalities.
- Tinel’s sign: Pressure and movement over the tarsal nerve tunnel to assess for nerve irritation.
Range of Motion and Strength
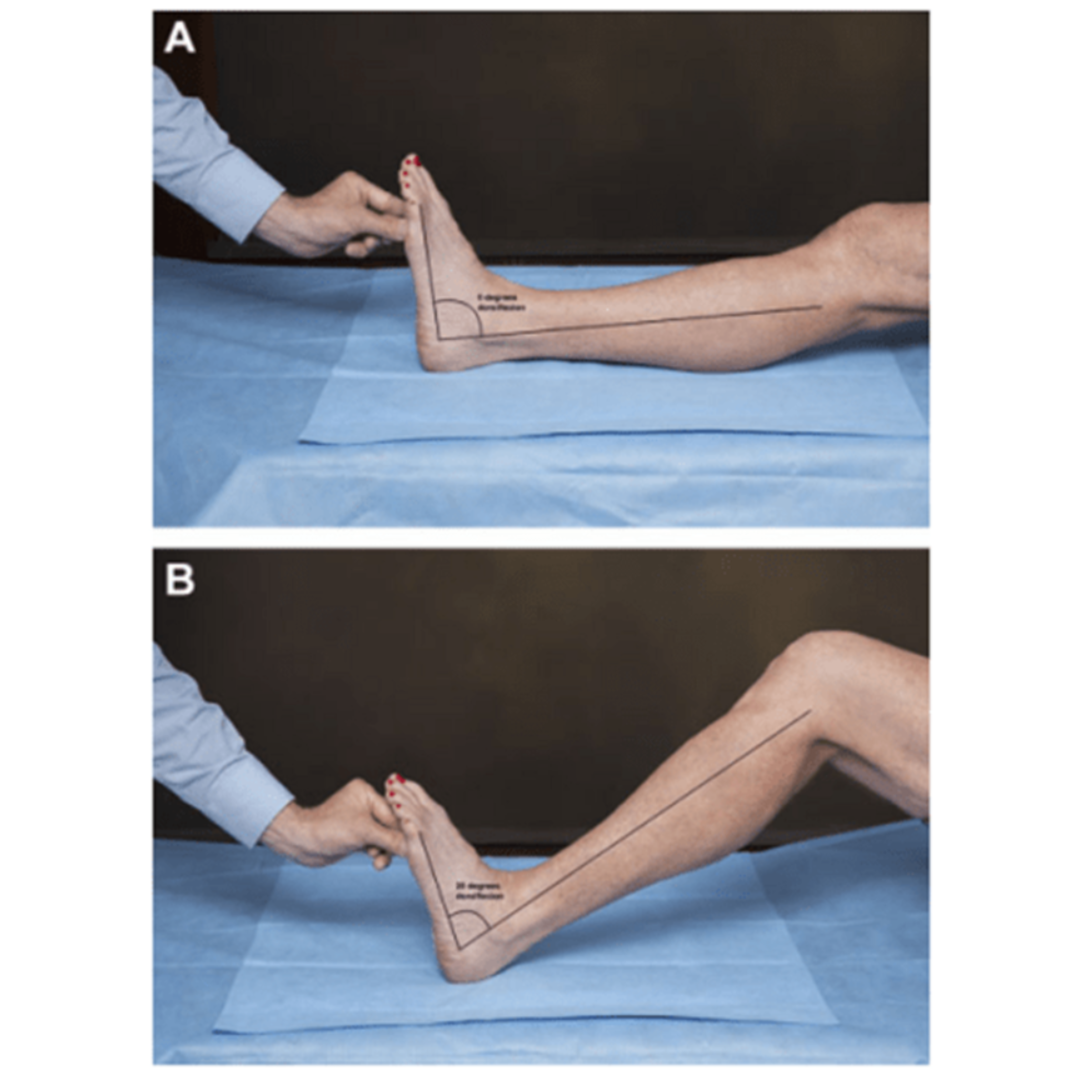
- Ankle dorsiflexion: Limited range may contribute to plantar fascia strain.
- Midfoot motion: Assess for restriction or hypermobility.
- Big toe extension: Evaluate for pain or limitation.
- Muscle strength: Test calf, internal foot, and peroneal muscles.
Functional and Gait Assessment
- Heel raise test: Assess for pain or weakness.
- Single-leg stance and squat: Evaluate balance and functional capacity.
- Gait analysis: Identify overpronation, altered stride, or compensatory mechanisms.
Special Tests specific to plantar fasciitis
Windlass Test
The Windlass test is a key diagnostic manoeuvre:
- Non-weight-bearing: With the patient seated and knee flexed, the examiner dorsiflexes the great toe while stabilising the ankle. Reproduction of heel pain is a positive test.
- Weight-bearing: The patient stands with the toes over the edge of a step; the examiner dorsiflexes the great toe. Pain at the medial heel is a positive result.
A positive Windlass test has high specificity but variable sensitivity for plantar fasciitis.

Tinel’s Sign
Percussion over the posterior tibial nerve at the tarsal tunnel elicits tingling or pain in cases of tarsal tunnel syndrome, helping to differentiate from plantar fasciitis.
Squeeze Test
Compression of the calcaneus may reproduce pain in stress fracture or fat pad pathology.
Functional and Gait Assessment
Biomechanical factors play a significant role in plantar fasciitis. Gait analysis, either clinical or using advanced motion-capture technology, can identify:
- Reduced ankle dorsiflexion
- Excessive pronation or supination
- Altered step length or cadence
- Weakness in calf or hip muscles
- Low or high arches
Gait analysis informs targeted interventions, such as orthotics, footwear modification, or physiotherapy for specific issues.
The problem with most gait analysis is that it focuses on a very specific area. For example Reduced ankle dorsiflexion or how high you can raise your foot, the minimum range of movement for an ankle is 90 degrees or what is described as Plantar Grade. Range of movement from plantar grade, 20 degrees past this point is good dorsiflexion pulling foot up and 50 degrees of plantar flexion pushing the foot down.
The root cause of plantar fasciitis in my experience is how you walk!
So to cure Plantar Fasciitis how you walk and stand need to be modified
At my clinic Energy Medicine all patients with Plantar Fasciitis go through this type of gait analysis importantly in bare feet.
Visual Observation
- We’ll watch you walk naturally in a straight line.
- We may ask you to walk for a more extended period outside in shoes.
- If relevant, we might observe you running as well.
Biomechanical Assessment
- We analyse the movement of your feet, ankles, knees, hips, and lower back.
- We look for any asymmetries or irregularities in your gait.
Foot Strike Pattern
- We observe how your foot lands (heel, midfoot, or forefoot).
- We check for overpronation or supination.
Stride Length and Width
- We measure the length and width of your steps.
- Abnormalities here can indicate compensation for pain.
Timing and Rhythm
- We assess the timing of each phase of your gait cycle.
- Irregularities can point to specific areas of discomfort.
Muscle Activity
- We observe which muscles are active during different phases of your gait.
- This helps identify any muscle imbalances or weaknesses.
Joint Angles
- We analyse the angles of your joints during movement.
- This can reveal issues with flexibility or joint function.
Pressure Distribution
- Observation to see how weight is distributed across your feet.
- This helps identify areas of excessive pressure that could contribute to plantar fasciitis.
Video Analysis
- We might record your gait for a more detailed analysis.
- Slow-motion playback allows us to catch subtle irregularities.
Footwear Assessment
- We’ll examine your shoes for wear patterns.
- This can provide insights into your typical gait patterns.
Treatments are initial readings with the interX Medical device to isolate pain points and start the treatment process. This gives a indication of the damage of the tissue of the fascia and helps inform the treatment plan going forward.
Conclusions and Treatment Plan
At the end of the Assessment a summary of key findings and solutions are presented to you and a treatment plan is outlined and explained.
Will you book an Initial Assessment and Treatment below?
