Well there are two very important issues with a Knee Replacement:
Can you fully straighten your Knee while standing and sitting so the joint can take full loading.
Can you bend it more than 90 degrees while standing on one leg?
Those are obviously essential for movement, but, are much more important post knee replacement surgery. Lots of things happen when you have knee replacement surgery as this is a complex joint with 4 major ligaments for support and 7 tendons for muscles the surgery team have to navigate.
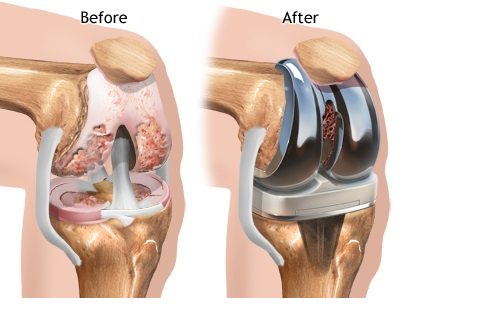
The primary reason for knee replacement is wear and tear with osteoarthritis. This means the cartilage wears away, so the joint is bone on bone and very painful. The knee replacement is metal plates inserted where the cartilage would normally be and attached. The surgery has a excellent success rate 99% and the majority after recovery are largely pain free.
The issue is movement, specifically range of movement!
Surgery varies depending on the wear and tear of the knee and can be operated on more in a straight position, or bent as required and this can have a impact on movement post-surgery. If it was operated on in a straight position standing and straightening knee is easier. If it was more bent when operated on bending tends to be easier.
This is most evident in the initial 6 to 8 weeks of recovery with stiffness and swelling, in some cases lots of swelling. So standing, sitting and walking has to be modified, with the added issue of using crutches and progressing to one crutch then no crutches.
The focus is zero and 90 degrees. This is usually ok with a bit of pushing to 90 degrees and zero is approximate so closer to 8-10 degrees so nearly straight. 6-8 weeks after surgery this is fine as people are still recovering as its major surgery and the inflammation will still not have fully gone.
The issue for knee replacements tends to start now.
You have usually stopped using crutches or sticks now and can move around home and do normal things getting in and out of bed, walking short distances, in and out of a car as you can drive, so able to go out. At this point you may consider to return to work and you feel great as the pain has gone swelling down and life is getting back to normal.
If you are in this situation right now or have had a knee replacement for some time try these two things:
- Firstly stand up using something for support and standing on your non operated leg raise your ankle behind you bending your knee aiming for 90 degrees. Have someone look if you cannot see, how does it feel easy or awkward?
- Secondly sit on the floor with your legs out straight in front of you. Now most people have tight backs of the legs the hamstrings, how do they feel behind the knee? After only a short period of time you will feel uncomfortable and your knees will want to bend upwards.
The reason for this is you have not recovered or specifically rehabilitated properly. You will probably have done the exercises regularly, initially ,but, not as much now and your body is still healing.
It is essential to keep pushing to fully recover as you are experiencing a false dawn due to the progress made post surgery.
Your knee should last at least 20+ years and you want to get full benefit from the surgery. I Help people get back to walking, running and doing a full range of activities with and extended range of movement so everything just works!
